Culture shift at UnitedHealth? Minnesota hospitals are wary
Published in Business News
UnitedHealth Group’s biggest public controversy in Minnesota a year ago was its fight with health systems threatening to leave the insurer’s Medicare network as contract negotiations stalled.
Now — with its air of invincibility punctured by federal investigations and financial missteps — the Eden Prairie, Minnesota-based health care giant is striking a conciliatory tone, including a pledge for friendlier relations with hospitals and clinics.
They’re going to need to be convinced.
“Minnesota hospitals have long struggled with UnitedHealth and its subsidiaries regarding prior authorizations and reimbursements for care,” the Minnesota Hospital Association said in a statement. “The company has, in the past, shown limited interest in responding to concerns about these issues.”
The reaction illustrates a trust gap built over years.
UnitedHealth Group has consistently generated billions in profits while managing finances for a wide swath of the U.S. health care system. Meanwhile, the hospitals’ trade group said, providers often struggled to have insurance claims pre-approved and, ultimately, paid by the company’s insurance unit, UnitedHealthcare.
CEO Stephen Hemsley vowed this week to reposition the nation’s largest health care company to become easier to work with, more reliable and consumer-friendly.
It’s not just hospitals and clinics that are wary; so is one of UnitedHealth’s largest business partners: the federal government.
The company this month acknowledged a Justice Department probe into allegations that it has gamed Medicare Advantage by using diagnosis data to wrongly boost risk-based payments.
The investigation comes as UnitedHealth faces unprecedented financial challenges while still earning billions.
Hemsley told investors this week that his company has embarked “on a real cultural shift in our relationships with regulators and all external stakeholders.”
“We intend to be proactively engaged, constructive and responsive to the concerns of all stakeholders and in our engagement with them,” he said.
“We have the chance to reposition our enterprise as a far more modern, reliable, consumer- and provider-friendly enterprise.”
It’s unclear where trust and culture rank on Hemsley’s to-do list. He returned to the top job in May after having previously held it during a period of tremendous growth between 2006 and 2017.
Relations with health care providers have been strained, including contract disputes last year in which two large health systems in Minnesota alleged wrongful denial of claims and payment delays by UnitedHealthcare.
Minnesota clinic operators say they watched a high-profile coverage conflict this year between UnitedHealth and a Texas surgeon, and felt a kinship with the physician, who commented in a widely watched social media video: “It’s 2025, and insurance just keeps getting worse.”
UnitedHealth denied the allegations and defended its practices in all cases.
Some tension is inevitable because insurers are supposed to scrutinize claims from health care providers, said Jonathan Weiner, a professor of health policy and management at Johns Hopkins Bloomberg School of Public Health.
Not all treatments that a provider or patient want fit within clinical guidelines, Weiner said, and U.S. private insurers are tasked with restraining the growth of health care budgets. That’s why insurers impose requirements, for example, that some treatments receive prior authorization.
Patients and doctors are bound to be unhappy with anyone saying “no,” Weiner said.
Limited federal data suggests denials might be more common at UnitedHealthcare than other insurers. The company insists those figures are “grossly misleading” because the data includes a small fraction of UnitedHealth’s total enrollment.
Navigating tensions with health care providers and other stakeholders is part of the challenge for insurance company executives.
“UnitedHealth Group leadership’s recent proclamations are likely one part mea culpa — indicative of a real desire for positive change — one part desire to stave off government regulators and one part PR marketing," Weiner said. “Time will tell which of these motivations will dominate.”
The company realized a profit of $3.4 billion from operations between April and June, short of investor expectations. It also revealed medical costs will soar $6.5 billion higher than anticipated among its 50 million insurance members.
UnitedHealth Group employs about 400,000 people worldwide, including about 19,000 in Minnesota.
The return of Hemsley, an accountant by training, signaled to many that UnitedHealth Group intends to tightly focus on the numbers.
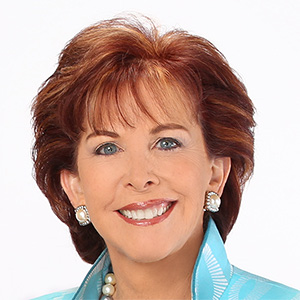
Even so, Dr. Archelle Georgiou, a one-time chief medical officer at the company, told the Minnesota Star Tribune in May that she expected Hemsley to prioritize culture issues while addressing frustrations that have tarnished UnitedHealthcare’s reputation with providers.
Hemsley began his comments Tuesday by thanking workers and describing the tone he wants the company to set.
Building trust is not simply a worthy goal, a former company executive said this week. It’s also imperative if UnitedHealth Group wants to avoid the government breaking up the company as it did in the past with such behemoths as Bell Telephone and Standard Oil.
“Stephen Hemsley, given his stature and history with the company, is the only person who could lead this kind of change,” the former executive said.
“Focusing narrowly on quarterly profits, financial engineering, growth at all costs, aggressive denials and gaming government payments for Medicare Advantage is no longer a winning strategy.”
The Wall Street Journal reported last year that the Justice Department had opened an antitrust investigation. The revelation of the criminal probe came this year.
Minnesota health care providers are watching because UnitedHealthcare has grown from having no Medicare Advantage enrollment in the state during 2018 to the third-largest in the local Medicare Advantage market last year.
The ranking still holds, even though UnitedHealthcare lost about 8,000 enrollees going into 2025 following contract disputes with Bloomington-based HealthPartners and Duluth-based Essentia Health. Those disputes were ultimately resolved.
“We hope the company is genuinely interested in a cultural change,” the Minnesota Hospital Association said.
©2025 The Minnesota Star Tribune. Visit at startribune.com. Distributed by Tribune Content Agency, LLC.









Comments