Mayo Clinic will leave most Medicare Advantage networks at UnitedHealthcare, Humana
Published in Business News
Mayo Clinic will go out-of-network next year for most Medicare Advantage plans from two of the nation’s largest health insurers.
The changes, which UnitedHealthcare and Humana confirmed over the past week to the Minnesota Star Tribune, mean tens of thousands of beneficiaries in Minnesota will need different insurance coverage if they want to retain access to the marquee medical center.
Neither Mayo nor the insurance companies offered explanations for the change. Officials with the health care provider noted Mayo is already out-of-network nationally with most Advantage plans, which are a privatized form of Medicare coverage.
Humana issued a statement that alluded to a longstanding complaint among insurers and some employers about what they describe as the high cost of health care at Mayo.
“When providers require significantly higher reimbursement rates compared to original Medicare, it further strains our health care system,” the Kentucky-based insurer said in a statement.
Mayo officials said the clinic will continue to participate in original Medicare and stressed that “a substantial portion of the care we deliver each day serves patients with Medicare coverage.”
The network cuts at UnitedHealthcare and Humana are just two examples of how more than 1.1 million people in Medicare across the state are sizing up big changes for next year — from higher premiums to fewer choices — with this week’s launch of the annual Medicare shopping season. About 650,000 here are enrolled in Medicare Advantage plans, and the rest have original Medicare, which is often supplemented with add-on coverage purchased in the private market.
Open enrollment runs from Oct. 15 through Dec. 7.
The federal government is projecting the average insurance premium for Minnesotans will increase nearly 18% next year in the plans.
And as costs are rising, Minnesota is seeing the second-largest drop across all states in the number of plans available next year, with the average beneficiary seeing 11 fewer options, according to a report this week from California-based health care research group KFF.
Provider networks are an important limitation with Medicare Advantage coverage.
Enrollees in these plans who use an out-of-network hospital or clinic might face much higher out-of-pocket costs or, as with Mayo, they could be blocked from scheduling appointments altogether.
The change at Minnesota-based UnitedHealthcare, which is the nation’s largest health insurer, starts Jan. 1 for people enrolled in the company’s Medicare Advantage plans for individuals. It does not apply to seniors in employer group Advantage plans for retirees.
People who get UnitedHealthcare coverage through their work are among those not affected.
“We have reached a multi-year agreement that provides continued network access to Mayo Clinic for people enrolled in UnitedHealthcare employer-sponsored commercial plans and Medicare Advantage Group Retiree plans,” the company said.
Medicare Advantage plans tend to have lower premiums compared to what it costs to get original Medicare plus any recommended “Part D” plans for prescriptions and Medicare Supplement coverage. One of the tradeoffs for lower premiums with Medicare Advantage is that some plans restrict access to certain doctors and hospitals.
There was a time when Minnesota seniors with Medicare Advantage coverage could use out-of-network benefits to visit Mayo. But the hospital system made changes to stop scheduling visits for these patients starting in 2022.
The scheduling block has made it even more important for beneficiaries to check the network of different Medicare Advantage plans during open enrollment if they want access to Mayo.
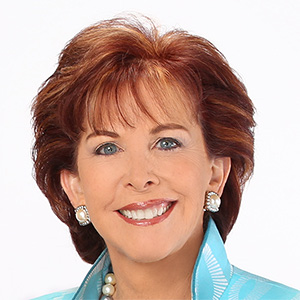
“People in Minnesota — so many of them want to be able to go to Mayo," said Kelli Jo Greiner, the Medicare program director at the Minnesota Board on Aging. “It’s a question people ask us; they want to know what plan they can sign up with and be able to go to Mayo.”
In 2025, five Medicare Advantage plans across the state provide in-network access to Mayo. Next year only two insurers — Blue Cross and Blue Shield of Minnesota and Medica — will do so.
Mayo has long been criticized as a high-cost health care provider relative to other clinics and hospitals in Minnesota. The clinic has countered that critics fail to credit how Mayo’s high quality drives overall savings, including for sophisticated purchasers like Walmart.
Medicare Advantage plans across the country are facing increased cost pressures this year, but it’s too soon to say if that’s driving diminished access overall to high-profile medical centers like Mayo, said Jack Hoadley, a research professor emeritus in health policy at Georgetown University.
In the mid-Atlantic, UnitedHealthcare has been engaged for weeks in a public feud over contract terms with another marquee medical center, Baltimore’s Johns Hopkins University, whose providers are currently out of the network, Hoadley said.
But a search of United’s online provider directory shows other high-profile medical centers nationally remain in-network.
Contract negotiations are private but typically include arguments about the prices for services and the use of prior authorization to access care.
This year, UnitedHealthcare and other health insurers have talked about controlling Medicare Advantage costs in 2026 by offering more HMO plans, which don’t always cover specialist services without a referral from a primary care doctor.
They’re also making patients pay a higher share of the total bill, which discourages use of out-of-network hospitals and clinics.
With major medical centers like Mayo, Hoadley said, patients with fairly routine health care needs might note the clinic’s reputation and seek care there even when others could provide comparable quality at a lower cost. Original Medicare with a good Medicare Supplement policy lets seniors make such a choice, including duplicative care, without financial consequences.
“Does that lead us to getting too much care?” he asked. “Should a plan help to manage those decisions for us?”
For now, insurance agents say the clear trend is for Medicare Advantage plans to limit patient options.
“They’re simply closing their (broad-access plans) altogether or removing them from certain counties,” said Joshua Haberman, the chief executive at Alexander & Haberman in Bloomington, Minnesota. “Other companies are taking a different approach, where ... [these plans] function as much narrower networks.”
©2025 The Minnesota Star Tribune. Visit at startribune.com. Distributed by Tribune Content Agency, LLC.








Comments