Commentary: Katrina was bigger than a hurricane
Published in Op Eds
When Hurricane Katrina touched down near New Orleans 20 years ago on Aug. 29, 2005, I was just beginning my journey as a first-year medical student. I remember watching the footage of families stranded on rooftops, hospitals submerged, and the bodies of people and pets floating in the floodwaters.
I had not yet developed the language of public health or trauma-informed care, but I felt that something bigger than a hurricane had happened. I didn’t know then that my future patients — many of them plagued by poverty, violence and environmental injustice — would share similar pathology to the survivors.
Today, as an addiction medicine physician, I care for patients whose lives are shaped by trauma, displacement and loss. Many of them were children at the time of the hurricane. As adults now, they speak of depression, abandonment and the silence of our systems that failed to ask how they were doing. “They just wanted us to survive,” said one of the interviewees in the 2022 documentary film “Katrina’s Babies.” But surviving isn’t the same as healing.
Katrina was not only a climate catastrophe. It was also a mental health emergency. In its wake, studies revealed spikes in PTSD, depression and substance use among evacuees. The disaster helped accelerate the overdose epidemic, a public health crisis that rages on to this day.
Clinics and recovery centers were destroyed. Providers were displaced. Support systems disappeared. A study of low-income mothers affected by Hurricane Katrina found that nearly half met the criteria for PTSD and 12 years later, one in six still exhibited symptoms that met criteria for the diagnosis. Another study linked displacement to increased drug use among survivors. Parents, workers and youth struggle to cope in the absence of care.
And the disasters keep coming. Wildfires in California. Heat waves in Phoenix. Hurricanes in North Carolina. As climate disasters become more frequent, so does the trauma.
In poorly resourced communities, especially Black and brown ones, disaster recovery often means rebuilding roads before rebuilding lives. When trauma is untreated, substances become survival tools. When care is disrupted, recovery becomes unreachable.
If we are serious about ending the overdose crisis, we must prepare for trauma the way we prepare for storms. That means funding long-term, culturally grounded behavioral health services, embedding addiction and mental health professionals into disaster response teams. We must ensure access to medication-assisted treatment and harm-reduction tools, listening to and uplifting community wisdom in recovery planning.
This year, the 20th anniversary of Hurricane Katrina falls just two days before International Overdose Awareness Day (Aug 31), and the kickoff of National Recovery Month in September. It’s more than symbolic. It’s a reminder that climate trauma and addiction are intertwined, and recovery must be intersectional.
“Katrina’s Babies” reminds us that the children of that storm are now adults, many raising families, working, grieving and striving. Some are still fighting for stability. And some are gone.
As a young medical student, I learned that healing takes more than medicine. As a physician today, I know it takes justice.
Let’s not wait for the next disaster to act. The levees may have broken 20 years ago, but our obligation to rebuild with care, dignity, and equity remains.
_____
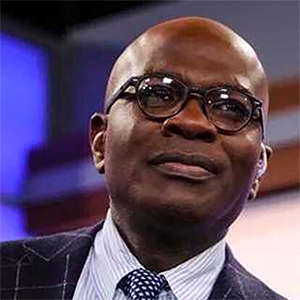
Audrey Tanksley is a double board-certified physician in internal medicine and addiction medicine and co-founder of Onyx Medical Wellness, which offers a patient-centered approach to address chronic disease, mental health and addiction. This column was produced for Progressive Perspectives, a project of The Progressive magazine, and distributed by Tribune News Service.
_____
©2025 Tribune Content Agency, LLC.




















































Comments