Commentary: We need an urgent and unified response to the coming Alzheimer's crisis
Published in Op Eds
In the early 1980s, men and women in the prime of their lives began arriving at Walter Reed Medical Center, wrecked by a disease for which we had no name, no cause and no hope. As an infectious disease doctor there, I saw patient after patient bedridden and dying by the time they reached my care.
Those early stages of the AIDS epidemic were marked by fear, confusion and stigma. Some doctors were even afraid to tell patients when they tested positive for the virus. It took years to understand what was happening, to learn that HIV infection was not merely a risk factor for AIDS, but the same disease at an earlier stage, and to encourage researchers to develop the multiple therapies necessary to control the disease. Now we know that HIV can be a manageable chronic condition when treated, and people with HIV can live normal lives without becoming critically ill. We know this because the federal government took decisive action to match our scientific understanding with a coordinated response and to focus on early disease and its timely diagnosis.
Today, the generation that survived that crisis is aging into the next public health emergency. Alzheimer’s disease affects more than 7 million Americans, and cases are expected to nearly double by 2050. We have poured billions of dollars into scientific research and medical innovation already. We know enough to lay the groundwork for a national response to Alzheimer’s and reduce suffering for millions — it must be based on early diagnosis at the beginning of the disease process. By learning from the AIDS epidemic, we can bring about the day when Alzheimer’s is no longer a death sentence but a manageable condition.
Just as undetected HIV yields the devastating symptoms of AIDS, Alzheimer’s has a silent phase that leads to the symptoms of cognitive impairment and loss of function. During this silent phase, which can last 20 years, amyloid proteins in the brain begin to misfold and clump into neuron-killing plaques. Recently, scientists discovered that these plaques can be accurately detected in the blood. The Food and Drug Administration this year approved a blood test for Alzheimer’s that showed greater than 90% accuracy in clinical studies. Researchers are now using similar tests in clinical trials to identify people even before overt symptoms appear. These tests fundamentally change our understanding of the disease, just as the HIV test did for AIDS.
The question of when Alzheimer’s begins is not a theoretical one. It sets the starting line for diagnostics and treatment options. Earlier detection means more opportunity for early-stage interventions, which can extend independence and quality of life for people living with Alzheimer’s. We now have two FDA-approved anti-amyloid therapies shown to slow cognitive decline when used soon after symptoms start. They are now being studied before symptoms appear, which researchers call preclinical Alzheimer’s. In addition, recent research has shown that a mix of better nutrition, exercise and blood pressure control can measurably improve cognitive health.
Just as the federal government took coordinated action as HIV/AIDS science evolved, we need an urgent and unified response to the coming Alzheimer’s crisis. The road map is largely a matter of updating policy to match the current science.
The government should begin by endorsing what the FDA has already stated— that Alzheimer’s begins when amyloid becomes abnormal in the brain, decades before symptoms arise. The FDA calls this phase before symptoms Stages 1 and 2 of Alzheimer’s disease. Every public health agency should recognize this starting line and set policy accordingly. Such unified recognition can reduce stigma and inspire action, as it did with AIDS.
It can also expand access to early detection and treatment, so millions of aging Americans have options during the early window when intervention is most effective. If new tests and therapies for Alzheimer’s disease prove effective even before symptoms appear, and they generate solid evidence in gold-standard scientific studies, they should be approved without delay. At the same time, the Centers for Medicare & Medicaid Services should amend its national coverage determination for Alzheimer’s to include treatments for Stages 1 and 2 of Alzheimer’s disease.
CMS should also remove the coverage with evidence development (CED) requirements that it has singularly applied to Alzheimer’s treatments. CED is redundant to FDA approval and restricts access. Removing it for Alzheimer’s therapies will benefit asymptomatic and early-stage patients, who need these therapies to extend meaningful years with their loved ones. Removing CED would also encourage innovators to pursue other treatment avenues, accelerating the next breakthrough.
Over my career, nothing has been more powerful than witnessing the transformation of HIV/AIDS from a death sentence to a chronic, treatable condition. We have the chance to do the same with Alzheimer’s.
History will judge us by whether we apply hard-won lessons or ignore them. Either we get ahead of this crisis or watch a generation of Americans be swept into the devastating grip of disease. We must act urgently.
____
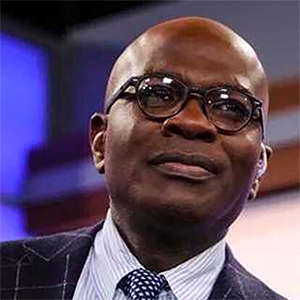
Dr. Robert R. Redfield, a former Centers of Disease and Control Prevention director, spent 20 years at Walter Reed Medical Center. He is associate director of the Institute of Human Virology at the University of Maryland School of Medicine.
___
©2025 Chicago Tribune. Visit at chicagotribune.com. Distributed by Tribune Content Agency, LLC.




















































Comments