UnitedHealthcare, Johns Hopkins fight over health insurance contract
Published in Business News
Doctors at Johns Hopkins Medicine hospitals and facilities could stop accepting insurance from national health insurance provider UnitedHealthcare in about a month if an agreement to maintain the health plan is not reached.
Just under 60,000 patients on UnitedHealthcare plans see Hopkins providers in Maryland, Virginia and Washington, D.C.
The medical system and the insurer have been negotiating contract updates for seven months, with an extension until Aug. 25.
The parties said they’ve agreed to medical care reimbursement rates but have clashed on language over prior authorization requirements and treatment denials. The current agreement has been extended five times during the past seven months.
In a July 25 update to patients, Johns Hopkins said it objects to “practices that put United’s bottom line ahead of your well being” and warned that without an updated contract by the deadline United could reduce or stop coverage.
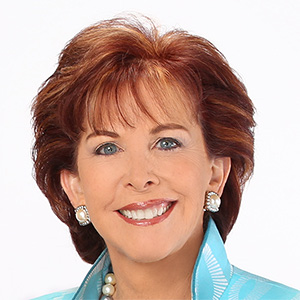
“Unfortunately, UnitedHealthcare has chosen to slow down negotiations recently because we refused to accept their harmful practices that hurt patients: aggressive claim denials that delay necessary care, excessive red tape that forces patients to wait for treatments, and significant payment delays that strain our ability to provide care,” Kim Hoppe, a Johns Hopkins Medicine spokeswoman, said in an email.
If no agreement is reached, patients in ongoing treatment for serious or complex conditions at a Johns Hopkins facility or from one of its physicians would be eligible for continuity of care, United said. That would apply to patients with conditions such as cancer or who are pregnant and who would be charged in-network rates until their treatment concludes.
But Johns Hopkins hospitals and facilities would be out-of-network for most patients, effective Aug. 25, without an agreement.
“Our top priority is to reach an agreement that maintains continued, uninterrupted network access to Johns Hopkins,” Joseph Ochipinti, UnitedHealthcare CEO for the Mid-Atlantic, said in an emailed statement. “Our negotiation isn’t about money.”
Frustrations over health insurance denials and medical bills made national headlines last December after the killing of UnitedHealthcare CEO Brian Thompson in Manhattan. Maryland native Luigi Mangione was indicted in April on a federal murder charge in Thompson’s killing.
Some of United’s in-network physicians and hospitals include Baltimore Washington Medical Center, Franklin Square Hospital Center, Harbor Hospital, Maryland General Hospital, Mercy Medical Center, St. Agnes Hospital, Union Memorial Hospital and University of Maryland Medical Center.
Emergency services would be covered at the in-network benefit level, regardless of whether the hospital participates in UnitedHealthcare’s network.
The contract applies to people enrolled in employer-sponsored commercial plans, individual Family Plans, Medicare Advantage plans, including Dual Special Needs Plans, and Group Retiree Medicare.
Johns Hopkins physicians do not currently participate in United’s Medicare Advantage or Medicaid networks. Johns Hopkins provider locations in Florida would remain in United’s network regardless of the outcome.
“We know your relationship with your doctors are deeply personal and important,” United said on its website. “We recognize and value the care Johns Hopkins provides and are committed to reaching an agreement that maintains continued network access to the health system.”
Hopkins said it disagrees with what it believes to be “barriers” to care, including excessive prior authorization requirements that can delay treatment, frequent treatment denials leading to appeals, administrative burdens and delayed payments.
Hopkins Medicine currently has “millions of dollars in unpaid claims” that have been submitted, the system said.
United said Hopkins has requested unacceptable contract provisions.
“Johns Hopkins is demanding language in its contract that would give them the right to refuse treatment for any employer it does not want to do business with,” the insurer said on its website. “They are attempting to reserve the right to turn away UnitedHealthcare members at their discretion as an in-network provider.”
UnitedHealthcare said it negotiates about 2,000 provider contracts each year, most of which are renewed.
Hopkins said it plans to keep patients updated on negotiations and will notify them of any changes in coverage. The insurer recommends members call the number on their health plan ID card for more information about how to apply for continuity of care and for questions or help finding alternative providers in their area.
©2025 The Baltimore Sun. Visit at baltimoresun.com. Distributed by Tribune Content Agency, LLC.









Comments