To treat a common bladder condition, Medtronic implant goes under the skin near the ankle
Published in Business News
To make life easier for people with a common bladder condition, Medtronic is digging in far away from urinary tract.
Treatment for urinary urge incontinence can require pads, absorbent underwear and medications that come with bothersome side effects. The Minnesota-run medtech firm’s tiny new implant, designed to help patients forget about their condition, goes under the skin of the ankle.
The Altaviva device, which recently received approval from the Food and Drug Administration after clinical trials began in April 2021, stimulates the tibial nerve to curtail patients’ sudden urge to urinate. It’s about the size of two chiclets.
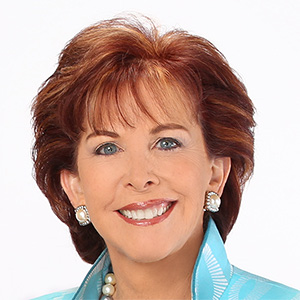
“We’ve been in this space for 30 years,” said Emily Elswick, president of the pelvic health business, about using mild electric stimulation to treat the condition. “And I think this is really going to help write a new book in this space — not just a new chapter, but a new book."
While Altaviva marks the first time Medtronic is stimulating the tibial nerve with an implant, the device builds on decades of advances in stimulating nerves to treat conditions such as Parkinson’s disease.
The FDA granted Altaviva approval last month after more than a year in review. The company is getting the word out on more 7,000 billboards to reach a patient population that CEO Geoff Martha called a “huge market.”
“We’ll take market share, which will be fun,” Martha said on a recent call with analysts. “But the bigger thing: We’re going to grow this market like crazy.”
BlueWind Medical’s Revi device works similarly, although patients with this device use an external wearable sleeve to activate the implant.
Dr. Kevin Benson, a urogynecologist at Sanford Health and investigator for the Altaviva device’s pivotal study, said the condition occurs when sensory wiring in the bladder wall that should normally be quiet becomes overactive. This results in the sudden urge to urinate, and patients have trouble reaching the restroom quickly enough, he said.
Elswick said the condition can feel shameful and embarrassing.
“A lot of them don’t want to talk about it,” Elswick said. “They’re afraid. Or they just don’t know where to go to seek treatment.”
Wearing pads has long been the standard of care, Benson said, forcing patients to “essentially compromise your life to live with a problem.”
Patients might have a hard time staying on medicines treating urge urinary incontinence, Benson said, as the drugs can cause dry eyes, dry mouth, constipation and could increase the risk of dementia. Doctors worry especially about that last point
A separate treatment called tibial nerve stimulation requires patients to return to the doctor’s office frequently through 12 weeks for health care providers to stimulate nerves by inserting an energized needle into the ankle, Benson said.
Former Medtronic CEO Omar Ishrak had previously urged the pelvic business to bet on expanding into tibial nerve treatments near the end of his tenure, which wrapped up in 2020, said Matt Stonehouse, vice president of research and development at Medtronic Pelvic Health. That resulted in the start of the Altaviva project. The implant’s development, largely based at the company’s Rice Creek facility, kicked off during the pandemic.
“We had to figure out how to do research and development during a time when the world was a little bit upside down,” Stonehouse said.
The result of that R&D is a silver implant marked by an active electrode and a return electrode, where energy streams into the ankle. In part, the device builds on a prior Medtronic implant inserted in the lower back stimulating the sacral nerve. But unlike its predecessor, Altaviva doesn’t have wires administering the stimulation.
At the Rice Creek facility recently, Stonehouse used a prosthetic lower leg to demonstrate the procedure, which takes about 15 minutes once a patient is on the table. After making an incision of less than 2 centimeters on the inner ankle, he checked to see if he had reached the connective tissue called the fascia. Above this layer, he inserted a tool into the incision to create a pocket, and slid the implant in right under the skin.
The competitor’s device, Stonehouse said, goes below the fascia: “It’s just a more invasive procedure.”
Once the device turns on, which occurs before the patient leaves the office, it sends energy through the nerves to the bladder to regulate its wiring to better communicate with the brain.
The implant’s battery lasts 15 years and does not fade with time, Stonehouse said. Patients recharge it once or twice a year.
Medtronic will present the unpublished clinical results that led to Altaviva’s approval at a conference later this month, but Benson said the data will show “people liked it, did well and had very minimal complications.”
©2025 The Minnesota Star Tribune. Visit at startribune.com. Distributed by Tribune Content Agency, LLC.







Comments