Stem cells may offer new hope for end-stage kidney disease treatment
Published in Health & Fitness
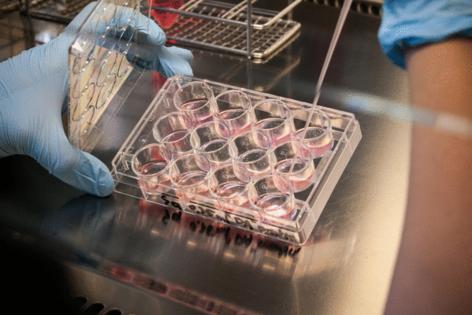
More than 4 million people worldwide have end-stage kidney disease that requires hemodialysis, a treatment in which a machine filters waste from the blood. Hemodialysis is a precursor to kidney transplant. To prepare for it, patients typically undergo surgery to connect an artery and a vein in the arm, creating an arteriovenous fistula (AVF) that allows blood to flow through the vein for treatment. However, AVF fails about 60 percent of the time due to vein narrowing. This is a major barrier to effective treatment.
Mayo Clinic researchers found that transplanting patients' own stem cells from fat cells into the vein often helped prevent inflammation and vein narrowing. This could help millions of people with end-stage kidney disease tolerate dialysis longer, extending the time before they require a kidney transplant.
That is because these adult stem cells called mesenchymal stem cells secrete healing growth factors that appear to be effective for certain patients with an AVF, according to Sanjay Misra, M.D., a Mayo Clinic interventional radiologist and senior author of the study published in Science Translational Medicine.
"Mesenchymal stem cells have anti-inflammatory properties," he says. "Inflammation is a significant problem, especially in Western society, because it's a hallmark of a lot of medical problems: heart disease, vascular disease, hypertension, high cholesterol and cancer. They are all driven by inflammation."
Dr. Misra collaborates with other physicians and researchers to explore stem cell therapies for a variety of diseases, from inflammatory bowel disease to osteoarthritis. However, his lab's primary focus is on the mechanisms that lead to the failure of hemodialysis graft, a surgical procedure that creates a permanent access point in the bloodstream for hemodialysis.
Improving kidney disease treatment options
In this study, 21 participants received AVFs as part of a phase I clinical trial. Eleven participants were injected with their own fat-derived mesenchymal stem cells before AVF surgery; 10 were part of the control group. The AVFs healed faster and were more durable in most of those who received the stem cells. However, not everyone responded to them.
"We were surprised by these differences in response to the mesenchymal stem cells. This spurred us to delve further into our research and include preclinical models and RNA sequencing technology," says lead author Sreenivasulu Kilari, Ph.D.
The researchers identified specific anti-inflammatory gene factors in those who responded well to the stem cells. They say these genetic biomarkers could help predict which patients are most likely to benefit from this stem cell application and help inform personalized treatment options. The researchers hope to garner more information through larger clinical trials.
©2025 Tribune Content Agency, LLC.






Comments